It was a surprise that health was devolved in Kenya’s 2010 constitution. The framers of the constitution were probably inspired by USA constitution where states have the mandate over health. The same happens in Canada. One of the missing links in our constitution is that we have two levels of government; county and national. Yet we borrowed a lot from USA which has a third level (counties) and middle level – states. The states are bigger but we seem to have given the counties the same mandate but with less resources. Compare California with 39 million (USA, 2020 Census) with Lamu which has about 154,774 in 2020(KNBS, 2020) but has the same mandate as California. Since USA constitution has amendments, maybe we need to amend ours too.
Back to health. One argument have heard is that health is so problematic that the national government was eager to devolve it to whoever wanted it! Health is comparable to tomatoes, very perishable. Once citizens are sick, you can’t wait. Tomatoes easily ripen and rot.
Apart from being a problem child, it’s not clear why health was devolved. May be doctors were too busy working to lobby for a commission like teachers.
How has heath faired in the devolved units?
Not as expected. A Kenya Devolution Sector CSO Working Group (KDCWG) study on Devolution @ 10 notes that despite some perceived improvements in health services due to increased county government investments, access to quality healthcare across various counties remains suboptimal with inadequate, inaccessible, and poorly managed health services. A disproportionate focus on curative over preventive services, limited resources, and infrastructure, management issues like corruption and political interference, and sociocultural barriers like traditional beliefs and lack of health education are identified as key deterrents to optimal health outcomes.
One problem has been that devolved units were not ready for this task. It takes a huge part of the budget. The skills shortage is another big challenge. Some counties like Nairobi have excess capacity, most medical schools are located there and students do not want to leave Nairobi after graduation. One curious observation is the number of jobless doctors and demand for doctors in some counties (Oketch & Shikanda, 2023).
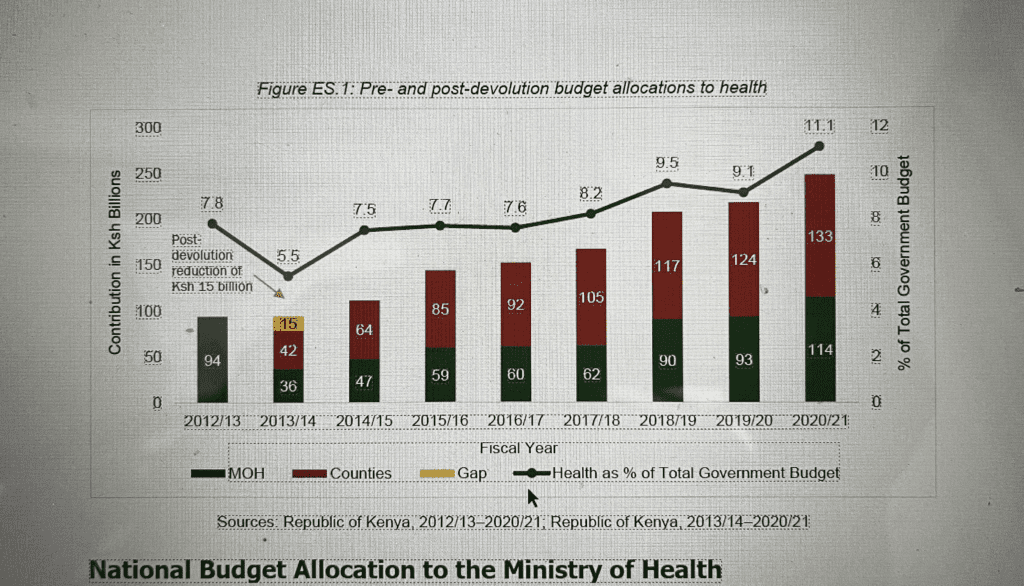
The second issue is that like other functions, the ministry of health has not let the counties go. Think of equipment leasing and Kenya medical supplies agency (KEMSA). There is too much centralization. That hampers efficiency and makes it hard for counties to get better deals. The bigger part of health budget is with the counties, but citizens still complain of access and cost particularly after shifting from national hospital insurance fund ( NHIF) to social health insurance fund (SHIF).
The paradox is that by devolving the health function, the economies of scale is hard to achieve. Perhaps counties need to talk to each other. Think Regional economic Blocks. Are there some functions they can share? Can they share specialists? Can they share labs? Mortuaries?
Third issue is data sharing. If a patient falls ill in one county, we have no reference to his prior health. Sharing data would make planning easier. Counties can even charge each other once we know where the patient hails. Availability of patient’s history would make diagnosis easier,particularly in case of emergencies.
Fourth, doctors and nurses strike is a symptom that all is not well in the county health systems. The call for a national health commission is another symptom. The devolution of major hospitals like Aga khan to the counties could be another symptom that health sector is not healthy in the counties. Add the frequent harambees to raise medical funds.
In the last 100 years the extension in life expectancy was driven largely by improvements in hygiene not advances in medical technology. The counties face lots of pressure to address non-communicable diseases like cancer, diabetes or heart diseases. The people who matter are likely to be victims of such diseases and hence get priority.
What percentage of health budget in counties goes to “modern diseases “compared with improvement in nutrition and clean water? What of mental diseases? Is this data available at county level?
Interconnectedness among key stakeholders will improve health. Bad roads make evacuation hard, lack of power lead to loss of essential drugs and lack of education keep superstitions alive and give business to herbalists and witch doctors. Poor nutrition and lack of clean water makes citizens prone to diseases. Sick citizens are not productive and the county economy falters. Use of gas to cook and electric cars could reduce respiratory diseases. Even simple things like house designs could make a difference to our health. Rural areas are heathier with plenty of fresh air and less pollution. Do counties encourage shift to rural areas?
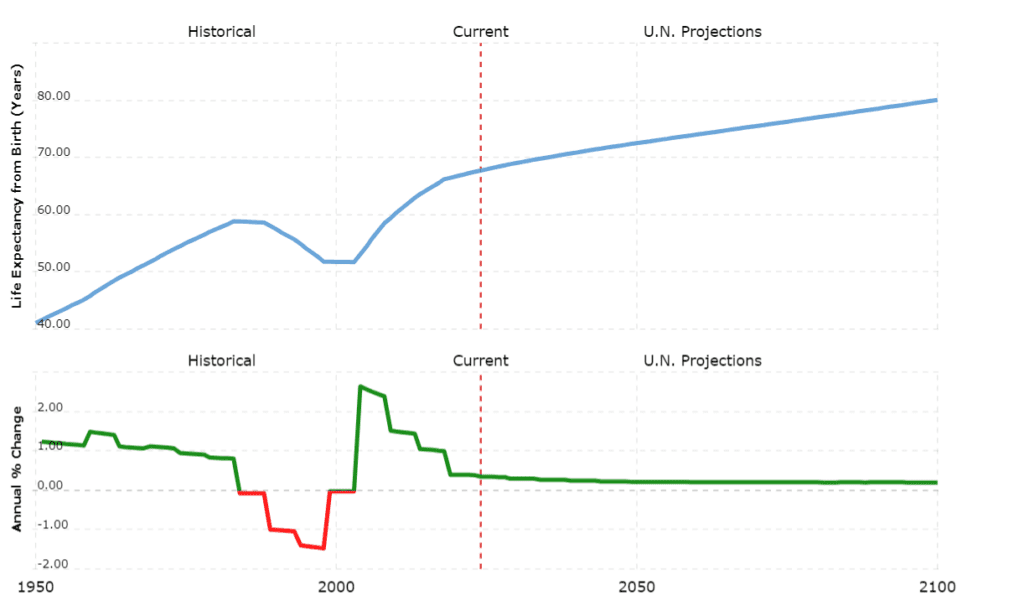
The ultimate test of county health is if life expectancy has goes up. Is data available by county and longitudinally?
Let’s go beyond counties into the macro environment.
Universal health coverage has been on the table since Uhuru government. We are now shifting from NHIF to SHIF. How will counties fit into the new insurance frameworks? How will the rural folks and urban poor be looped into this insurance?
Should health insurance be devolved so that each county has its own scheme to take care of the context? Pastoralists and urbanites have different health issues.
Let’s have more synergy. The national and county government should work together sharing resources, data and innovations. Private, public and mission hospitals share little. Could we add herbalists? What of counties themselves? What do they share? What of sports? With sports there would be less worry over obesity and heart diseases. Religion is a factor in health. Beyond reducing anxiety, it often keeps some away from modern medicine. Think of Akorino. Churches and other religious organizations also invest and own health facilities.
World Health Organization (WHO) has great policies on heath. How are they cascaded into grassroots and counties? Do the citizens feel them through better health?
What can we do to improve the health in the devolved units?
*Research: lots of hospitals are now “referral.” They should be centers of health research in the counties. How much of the country heath budgets goes to research? Lifestyle, climatic change and genetics have given us new diseases. Continuous research would help us address these new diseases. How much have we mapped our genes? Diseases like dementia and cancer were rare in rural areas. Why now?
*Climatic change has affected our health. Mosquitoes are now common in highlands. New species are thriving. How shall we deal with that? What of extreme heat? Dust? Floods?
* Incentives for doctors and nurses to stay in counties are needed. Housing? Ultimately, doctors are relocating back to the city because it has a conducive environment; another failure of devolution. One doctor who came back to Nairobi asked me “what shall I do in the countryside after work or over the weekend?”
* Let us look at the low lying fruits: our traditions were heathy. That’s is why we had no diseases of development. Traditional foods were nutritional and healthy. Remember food was boiled not fried. If fried, they used animal fat (healthier?)
*Real estate should focus on livability. Why do we crowd houses without parks and “breathing spaces.”?
*Sports are the golden route to better health. Do you recall walking and sports during Covid -19? Why didn’t we maintain that tempo? Why do we ignore sports after school? While we love premier league, why not sports over the weekend, and facilities are there. Every primary and high school has a field (stadium). Sport will improve our physical and mental health. They would keep us of from substance abuse too.
*Charity starts at home. What are the family traditions on matters of health? The staple food, hobbies, family harmony (for emotional health) and simple activities like kitchen gardening.
*School should teach the heath basics. Children remember. We brought cigarettes in class 5 and smoked through white handkerchiefs. The teacher then asked, “If the white handkerchief turns grey with one puff, what of your lungs if you smoke all your life?” Few of my classmates smoke.
* Educate citizens on health through media, and home visits. Focus on prevention. How effective is government 100, 000 health promoters?
* Create synergy with national government and other stakeholder’s .Eg. Would more optimistic media make us feel more emotionally healthy?
*Don’t re-invent the wheel. Learn from other countries and counties on how to improve health efficiency and effectively. Canada and Scandinavian countries are good benchmarks.
Conclusion
The youthful age of the Kenyan population may mask the heath issues particularly in the rural areas where the majority live. Through continues research we can unmask the health issues at the grassroots and address them and through one’s life cycle. Health is an input into our productivity and economic growth. That is not about to change.
REFERENCES:
Angela Oketch, A and Shikands, H (2023), https://nation.africa/kenya/news/the-frustrations-of-kenya-s-jobless-doctors-4111842 retrieved September 29th 2024.
KDCWG 2023: Devolution @ 10: A people’s perspective. Nairobi, Act Change Transform.
US census (2020), https://www.census.gov/programs-surveys/decennial-census/decade/2020/2020-census-results.html, Retrieved September 29th 2024.
XN Iraki is a Professor, Faculty of Business and Management Sciences, University of Nairobi.
@Kenya Devolution Program, Act Change Transform 2024